
How Herbal Medicine Shaped Modern Healing
Share
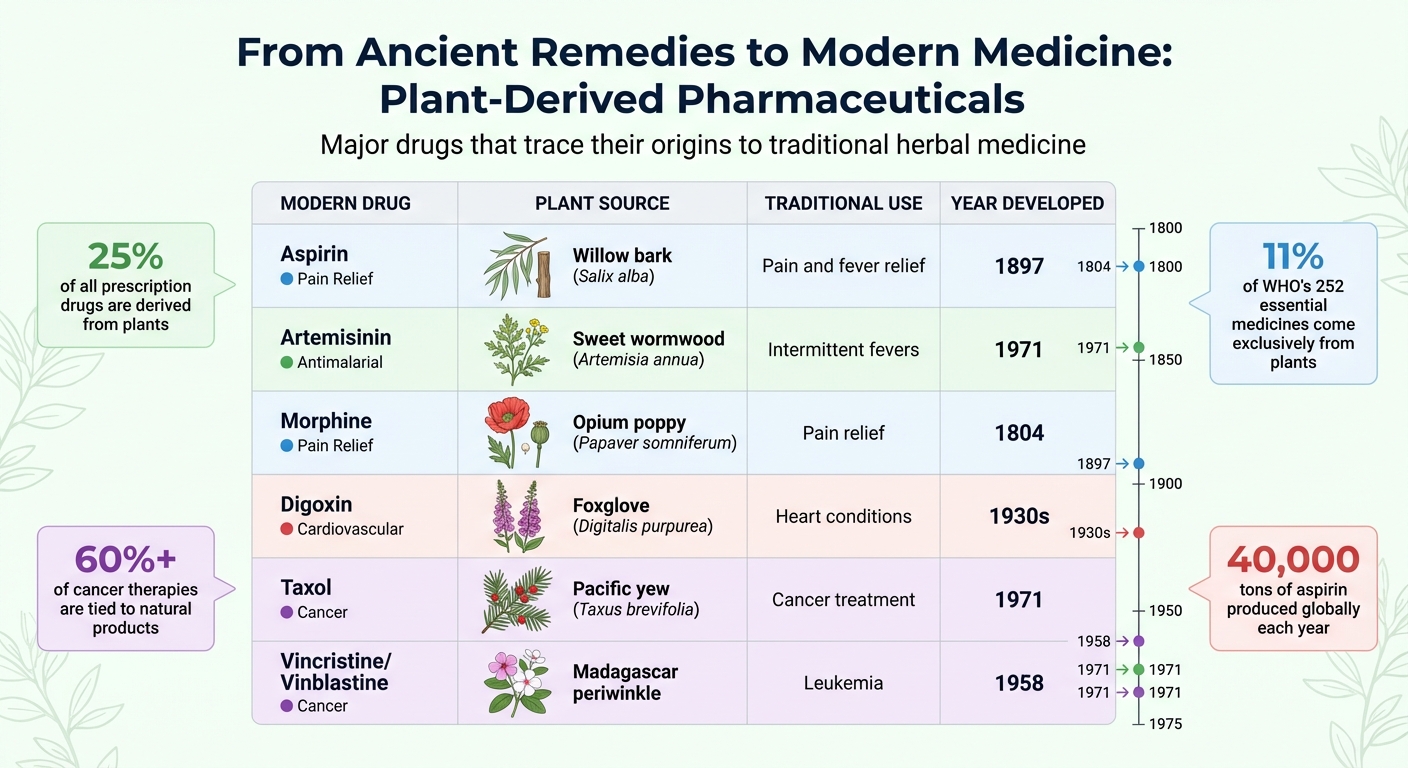
Herbal medicine has been central to healthcare for thousands of years, influencing modern treatments and pharmaceuticals. Ancient civilizations like Egypt, China, and India documented plant-based remedies, many of which are still in use. Today, around 25% of all prescription drugs are derived from plants, with notable examples including aspirin from willow bark and artemisinin from sweet wormwood. These traditional practices laid the groundwork for isolating active compounds, leading to modern drugs that treat conditions like cancer, malaria, and heart disease. Despite advancements, 80% of populations in some regions still rely on herbal remedies for primary care, highlighting their enduring relevance.
Key insights:
- Ancient texts like the Ebers Papyrus and De Materia Medica cataloged hundreds of plant-based remedies.
- Modern pharmaceuticals like morphine, digoxin, and Taxol trace their origins to plants.
- Herbal medicine continues to thrive, with the global market nearing $60 billion annually.
- Challenges include standardizing herbal treatments and addressing potential drug interactions.
The fusion of ancient knowledge with scientific validation has created a bridge between past practices and modern medicine, offering solutions for complex health issues.
The Origins of Herbal Medicine
Herbal Traditions in Ancient Civilizations
Herbal medicine has deep roots, with civilizations across the globe independently developing plant-based remedies. The Sumerians, as early as 3000 BCE, created the first known written records, listing 12 recipes that used over 250 plants. Their texts referenced plants like opium, poppy, henbane, and mandrake - many of which are still valued for their medicinal qualities today.
In Ancient Egypt, herbal medicine advanced further. The Ebers Papyrus, dating back to around 1550 BCE, contained detailed prescriptions. Egyptian healers frequently turned to garlic, aloe, castor oil, juniper, and cannabis to address various ailments. In China, the legendary text Shennong Ben Cao Jing, traditionally attributed to 2500 BCE, cataloged 365 medicinal plants, including ephedra, hemp, ginseng, and cinnamon. Similarly, India's Rig Veda and Atharva Veda (circa 1000 BCE) formed the basis of Ayurveda, mentioning turmeric, pepper, clove, and nutmeg. Later, the Sushruta Samhita from the 6th century BCE expanded this knowledge, describing 700 medicinal plants. Meanwhile, Ancient Greece formalized the study of plants with works like Theophrastus's Historia Plantarum in the 4th century BCE and Pedanius Dioscorides's De Materia Medica around 77 CE, which influenced medicine for over 1,600 years.
Indigenous communities in the Americas also developed extensive herbal practices, utilizing around 2,500 of the 20,000 plant species native to North America. While much of this knowledge was passed down orally, it reflected centuries of careful observation. Even Ötzi the Iceman, a 5,300-year-old frozen body found in the Ötztal Alps in 1991, carried birch polypore - a medicinal fungus likely used for treating intestinal parasites. These traditions, whether recorded or oral, formed the foundation for further medicinal discoveries.
How Herbal Knowledge Developed Over Time
Over the centuries, herbal medicine evolved through observation and experimentation. Early healers relied on watching animals interact with plants. For example, scientists have observed chimpanzees and sheep eating plants rich in tannins and alkaloids to rid themselves of parasites. These behaviors gave early humans valuable insights into which plants might have healing properties.
This trial-and-error approach allowed generations of healers to refine their remedies. Successes were remembered and passed down, becoming staples of herbal traditions. Evidence of this continuity can be seen in the Shanidar IV burial site, where pollen from eight plant species was found - seven of which are still used in herbal medicine today.
The advent of writing systems marked a turning point. Oral traditions transitioned into written records, enabling healers to document treatments, refine dosages, and build on existing knowledge. During the Middle Ages, European monasteries became hubs for preserving herbal wisdom. Monks cultivated medicinal herbs like sage, mint, and anise while meticulously copying ancient texts.
Even today, herbal medicine remains vital. According to the World Health Organization, 80% of the population in some Asian and African countries relies on herbal remedies for primary health care. This enduring reliance highlights the importance of centuries of observation, documentation, and refinement. These early practices laid the groundwork for modern pharmacology, bridging the gap between ancient remedies and contemporary medicine.
How Herbal Practices Led to Modern Medicine
Major Pharmaceutical Drugs Derived from Plants and Their Traditional Origins
Pharmaceuticals Derived from Plants
The connection between ancient herbal practices and modern medicine became clearer in the 19th century, when scientists figured out how to isolate active compounds from plants. This discovery allowed for more precise dosing and consistent treatments, laying the groundwork for clinical testing and validation.
For example, in 1897, Bayer chemists Felix Hoffmann and Arthur Eichengrün synthesized acetylsalicylic acid, better known as aspirin, from salicylic acid found in willow bark. For thousands of years, willow bark had been used to relieve pain and fever, but it often caused severe stomach irritation. The synthetic version kept the pain-relief benefits while greatly reducing side effects. Today, 40,000 tons of aspirin are produced globally each year.
Another groundbreaking moment came during China's "Project 523" (1967–1972), when scientist Tu Youyou led efforts to find a malaria treatment. Her team screened over 2,000 herbal remedies and turned to a 1,600-year-old text, A Handbook of Prescriptions for Emergencies by Ge Hong, which described using sweet wormwood (Artemisia annua) for intermittent fevers. Inspired by this ancient knowledge, her team successfully isolated artemisinin, which proved 100% effective in animal models at inhibiting malaria parasites. This discovery has saved millions of lives and earned Tu the 2015 Nobel Prize in Physiology or Medicine.
Here’s a closer look at some major plant-based drugs and their origins:
| Modern Drug | Plant Source | Traditional Use | Year Developed |
|---|---|---|---|
| Aspirin | Willow bark (Salix alba) | Pain and fever relief | 1897 |
| Artemisinin | Sweet wormwood (Artemisia annua) | Intermittent fevers | 1971 |
| Morphine | Opium poppy (Papaver somniferum) | Pain relief | 1804 |
| Digoxin | Foxglove (Digitalis purpurea) | Heart conditions | 1930s |
| Taxol | Pacific yew (Taxus brevifolia) | Cancer treatment | 1971 |
| Vincristine/Vinblastine | Madagascar periwinkle | Leukemia | 1958 |
Plant-derived products play a major role in modern medicine. About 25% of all pharmaceuticals are based on plant compounds, and 11% of the 252 drugs on the World Health Organization's essential medicine list come exclusively from plants. Even in cancer treatment, more than 60% of current therapies are tied to natural products.
Scientific Validation of Herbal Remedies
The journey from traditional herbal remedies to modern medicine wasn’t just about isolating compounds - it required rigorous scientific testing. One of the first documented clinical trials dates back to 1763, when English cleric Edward Stone tested pulverized willow bark on 50 patients with fevers. He found that 3.6 grams of the bark effectively reduced their fevers, providing a scientific basis for its use. Stone noted:
"many natural maladies carry their cures along with them, or that their remedies lie not far from their causes."
Today, validation involves far more than observation. Modern science uses controlled clinical trials to standardize plant extracts and ensure their safety and efficacy. In 2004, the U.S. Food and Drug Administration (FDA) introduced a "Botanical Drug" category to evaluate plant-based medicines under the same rigorous standards as conventional drugs. By 2018, the FDA had received over 800 botanical investigational new drug applications. So far, only two have been approved: Veregen (a green tea extract for genital warts) in 2006, and Fulyzaq (made from dragon's blood tree sap for HIV-related diarrhea) in 2012.
Researchers now use methods like ethnopharmacology - studying traditional uses of plants - and reverse pharmacology, which starts with traditional knowledge to guide drug development. This approach saves time by focusing on plants already known for their therapeutic effects. The World Health Organization highlights this connection:
"Around 40% of pharmaceutical products today draw from nature and traditional knowledge, including landmark drugs: aspirin, artemisinin, and childhood cancer treatments."
As Michael Wink from Heidelberg University explains:
"Herbal medicine is not a placebo medicine but a rational medicine, and for several of them clinical trials confirm efficacy."
However, challenges remain. Standardizing botanical products is tricky due to variations in factors like where the plant was grown, when it was harvested, and how it was processed. Ensuring consistency across batches is a crucial next step for herbal medicine to fully integrate into modern healthcare systems.
sbb-itb-9616115
Herbal Medicine in Today's Health Practices
Combining Herbal Supplements with Standard Medical Care
Integrative medicine brings together herbal remedies and conventional treatments to create a more comprehensive approach to health. In fact, 18.9% of adults in the U.S. turn to herbal products to address health conditions, making these remedies the most popular alternative therapy when prayer is excluded. This trend has even reached medical education, with the Consortium of Academic Health Centers for Integrative Medicine representing 44 institutions across the U.S. and Canada, actively working to incorporate herbal therapies into their curricula. Many people now use herbal products to support their overall health or help manage chronic conditions alongside traditional medical treatments.
But there's a challenge: only about 33% of people using herbal supplements inform their doctors about it. This lack of communication can lead to serious risks. For example, approximately 80% of prescription drugs are processed by six key CYP enzymes, and herbs like St. John's Wort and Goldenseal can interfere with these enzymes. Such interactions may cause toxicity or reduce the effectiveness of medications. This is especially critical for those taking anticoagulants, antidepressants, or cardiovascular drugs. If you're considering herbal supplements alongside prescription medications, it’s essential to talk to your healthcare provider and keep an eye out for potential interactions.
This growing use of herbal remedies is reshaping healthcare practices and fueling the demand for natural supplements.
The Growing Market for Natural Supplements
The herbal supplement industry has seen explosive growth, with U.S. sales surpassing $8 billion in 2017 - a 68% increase since 2008. This surge reflects a shift in consumer preferences toward natural therapies, as many people seek alternatives to synthetic medicines due to concerns about side effects. Globally, the herbal product market is nearing $60 billion annually, as consumers increasingly look for holistic solutions that address not just physical health but also psychological and spiritual well-being. Many also find natural supplements to be more accessible and affordable than costly prescription drugs.
Companies like Mahoney Supplements (https://mahoneysupplements.com) are stepping up to meet this demand. Their offerings include products such as ParaGon for parasite cleansing ($104.95), TUDCA & NAC for liver detox ($92.00), and B17 for immune health ($102.95). These supplements focus on natural ingredients and take a whole-body approach to wellness.
Scientific research further supports the value of herbal medicine. For instance, artemisinin’s discovery earned a Nobel Prize, and botanical derivatives like capsaicin have been clinically validated for treating neuropathic pain. When choosing supplements, consumers should look for third-party certifications to ensure quality and safety. And as always, consulting a healthcare provider before starting any new supplement is a wise step toward maintaining health and avoiding unintended interactions.
Conclusion
The evolution from ancient herbal practices to modern medicine highlights the powerful synergy between age-old plant knowledge and contemporary scientific research. Today, around 25% of all prescribed medications globally are derived from plants, with many cancer treatments tracing their origins back to nature. This blend of ancient wisdom and modern advancements is reshaping how we approach healing.
Modern scientists are increasingly turning to reverse pharmacology, where they start with traditional remedies and work backward to understand their effects. It’s a logical move when you consider that conventional drug discovery has a staggering 95% failure rate in clinical trials. As Timothy Mitchison from Harvard Medical School explains:
The long history of human data we have for traditional Chinese medicine could be the most valuable thing you can get to help characterize any drug.
This approach is further enhanced by cutting-edge tools like AI, genomics, and high-throughput screening. These technologies allow researchers to identify active compounds and decode how traditional remedies function at the molecular level. For example, scientists at Shanghai University of Traditional Chinese Medicine identified notoginsenoside Ft1 from Panax notoginseng - a plant with a 2,000-year history - as a promising treatment for obesity. Such advancements are unlocking the hidden potential of ancient formulas.
What sets this integration apart is its ability to address complex diseases. While modern pharmaceuticals often target a single compound, traditional remedies frequently use multi-compound formulas, making them more effective for conditions like diabetes, autoimmune disorders, and cancer. These remedies work on multiple biological pathways simultaneously, offering a more comprehensive approach to treatment. By combining traditional practices with rigorous scientific validation, we’re achieving outcomes that neither could accomplish alone.
The future of medicine lies in honoring and combining both traditions. Whether it's artemisinin saving millions of lives since 2000 or the untapped potential of other ancient remedies, this fusion of knowledge opens doors to groundbreaking therapeutic possibilities. From the roots of ancient practices to the forefront of scientific innovation, herbal medicine continues to shape the path of modern healing.
FAQs
How has herbal medicine influenced modern medicine?
Herbal medicine has been a cornerstone in the development of modern medicine, laying the groundwork for many of today’s pharmaceuticals. Traditional remedies often relied on plants rich in bioactive compounds, which researchers have studied, refined, and adapted into widely-used drugs. Take aspirin, for example - it originates from willow bark. Similarly, taxol, a well-known cancer treatment, was derived from the Pacific yew tree, while Vinca alkaloids, used in chemotherapy, come from the periwinkle plant. These examples show how age-old healing practices continue to influence advancements in healthcare.
Beyond pharmaceuticals, the influence of herbal medicine extends to the realm of natural health supplements. Companies like Mahoney Supplements draw on well-researched plant extracts to create products such as liver-support capsules (TUDCA + NAC), parasite-cleansing blends, and immune-boosting B-17. By combining traditional herbal knowledge with modern wellness trends, they offer natural options that aim to support health and overall well-being.
What challenges arise when combining herbal remedies with modern medical treatments?
Integrating herbal remedies with modern medicine isn't without its hurdles. One of the biggest challenges is the limited scientific evidence supporting many herbal products. This lack of robust research makes it tough for healthcare providers to assess their safety and effectiveness. On top of that, the absence of standardized manufacturing processes leads to inconsistent product quality. Variations in active ingredients and the risk of contamination can make it hard to trust the reliability and safety of these remedies.
Another pressing issue is the potential for herb-drug interactions. These interactions can alter how prescription medications work in the body, sometimes causing harmful side effects. Unlike prescription drugs, most herbal remedies in the U.S. are classified as dietary supplements. This means they don't go through the same rigorous pre-approval testing, leaving patients and doctors with little guidance on proper dosing or usage.
Cultural and systemic factors add another layer of complexity. In the U.S., herbal remedies are often viewed as complementary or alternative treatments, which can lead to uncertainty in clinical practice and challenges with insurance coverage. Compounding the problem, many healthcare providers lack formal training in herbal medicine, making it difficult for them to advise patients effectively. Overcoming these obstacles will require more extensive research, standardized product guidelines, and improved education for both medical professionals and patients.
Why is it important to scientifically validate herbal medicine?
Scientific research plays a crucial role in connecting traditional herbal remedies with modern medical practices. Through controlled studies, scientists can verify the effectiveness of various herbs, pinpoint their active ingredients, and determine safe usage guidelines. This process ensures that treatments derived from these plants are not only reliable but also consistent and safe for patients.
Moreover, validation paves the way for herbal remedies to become a part of mainstream healthcare by standardizing their quality and production methods. In fact, many well-known medications, such as aspirin and artemisinin, have roots in plants historically used in traditional medicine. For companies like Mahoney Supplements, grounding products like ParaGon, TUDCA & NAC, and B17 in rigorous scientific research guarantees their safety and efficacy, blending the principles of natural health with evidence-based science.
