
How Photobiomodulation Devices Work
Share
Photobiomodulation (PBM) uses specific wavelengths of red and near-infrared light to boost cellular energy, reduce inflammation, and promote healing. By targeting mitochondria - the cell’s energy center - PBM increases ATP production, releases nitric oxide, and triggers beneficial cellular responses. It’s non-thermal, painless, and works with your body’s natural processes.
Key Points:
- How It Works: PBM uses light to stimulate cytochrome c oxidase in mitochondria, improving cell function.
- Light Types: Red light (600–700 nm) for surface-level issues, near-infrared light (700–1,100 nm) for deeper tissues.
- Applications: Pain relief, wound healing, skin rejuvenation, and neurological support.
- Devices: Include handheld lasers, LED panels, wearable wraps, and full-body systems.
- Dosing Matters: Too much or too little light can reduce effectiveness; proper intensity and wavelength are critical.
PBM is backed by extensive research, making it a practical option for managing pain, improving recovery, and supporting overall health.
The Science Behind Photobiomodulation
How Light Interacts with Cells
Red and near-infrared light can penetrate deep into tissues, reaching the mitochondria inside your cells. At the heart of this process is an enzyme called cytochrome c oxidase (CCO) - a key player in your mitochondrial respiratory chain. This enzyme acts as the primary target for light absorption, thanks to its heme and copper centers.
In cells that are low on oxygen, nitric oxide (NO) binds to CCO, disrupting cellular respiration. However, when red or near-infrared photons hit these centers, they prompt the release of NO, especially under stress conditions. As Michael R. Hamblin, Ph.D., explains:
"The leading hypothesis is that the photons dissociate inhibitory nitric oxide from the enzyme, leading to an increase in electron transport, mitochondrial membrane potential and ATP production."
Once NO is released, oxygen can rebind to CCO, restoring the flow of electrons and boosting mitochondrial function. This process enhances the mitochondrial membrane potential and drives ATP production, giving your cells the energy needed for repair and regeneration. Interestingly, mitochondria account for about 50% of optical absorption in blood-free tissue at 780 nm, which is why metabolically active cells respond so well to photobiomodulation.
This interaction between light and mitochondria is the foundation for the cellular responses discussed below.
Cellular Effects of Photobiomodulation
After mitochondria are reactivated, cells respond quickly by ramping up energy production and initiating signaling pathways. This surge in mitochondrial activity fuels cellular repair and regeneration. Light absorption not only increases ATP production but also triggers a controlled burst of reactive oxygen species (ROS).
Although ROS are often associated with cellular damage, in small amounts they serve as crucial signaling molecules. These molecules activate transcription factors like NF-κB and AP-1, which then move to the cell nucleus to regulate genes involved in protein synthesis, cell migration, inflammation control, and antioxidant production. This process, known as mitohormesis, highlights how low levels of oxidative stress can actually lead to beneficial cellular adaptations.
For example, a study from March 2021 found that using a 980 nm diode laser at 0.8 W for 60 seconds (61.54 J/cm²) significantly boosted ATP production by stimulating Complexes III and IV in the mitochondrial respiratory chain. This demonstrates the biphasic dose response of photobiomodulation: the right dose promotes healing, while too little or too much may be ineffective or even harmful.
Beyond ATP and ROS, photobiomodulation also impacts nitric oxide release, which enhances blood flow through vasodilation, and triggers calcium influx via light-sensitive ion channels. Longer near-infrared wavelengths (900–1,100 nm) are particularly effective in activating these channels by interacting with structured water clusters on their surface. Together, these processes create a feedback loop between mitochondria and the cell nucleus, known as retrograde signaling, which explains why even brief light exposure can produce effects lasting hours or even weeks.
Key Parameters of Photobiomodulation Devices
To truly grasp how photobiomodulation works, it’s crucial to understand the key parameters: wavelength, penetration depth, intensity, and energy dose. These factors determine how light interacts with cellular processes, ultimately influencing the effectiveness of treatment.
Wavelengths and Penetration Depth
Light doesn’t penetrate tissue uniformly, and the wavelength you select dictates how deep the photons travel and which tissues they can affect.
- Red light (620–700 nm) scatters significantly as it passes through tissue, limiting its reach to about 1–5 mm beneath the skin. This makes it ideal for surface-level applications like skin rejuvenation, wound healing, and even hair regrowth.
- Near-infrared light (NIR) (700–1,100 nm) penetrates much deeper, ranging from 5–15 mm, allowing it to reach muscles, bones, and internal organs. For example, light at 810 nm can penetrate 2–10 mm, while 890 nm light can reach depths of 5–15 mm. This makes NIR particularly effective for muscle recovery, reducing joint inflammation, and addressing neurological issues.
However, wavelengths between 700 nm and 780 nm often fall short. This range coincides with a dip in the absorption spectrum of cytochrome c oxidase (COX), the mitochondrial enzyme that absorbs light. Devices operating in this range may yield inconsistent results. On the other hand, wavelengths near 665 nm and 810 nm, where COX absorption peaks, are far more effective.
Intensity and Energy Dose
Intensity and energy dose are often confused, but they’re not interchangeable. Intensity (measured in mW/cm²) reflects the rate at which energy is delivered, while fluence (measured in J/cm²) indicates the total energy delivered over time.
Photobiomodulation works according to the Arndt-Schulz Law, which describes a biphasic dose response: low doses stimulate cellular activity, while high doses inhibit it. Research backs this up. A 2005 study by Karu and Kolyakov found that DNA synthesis peaked at an intensity of 0.8 mW/cm², even when the total energy (fluence) was held constant at 0.1 J/cm². Similarly, another study by Orion and colleagues observed that rat heart tissue responded best at 5 mW/cm², but benefits dropped at both 2.5 mW/cm² and 25 mW/cm². This highlights the importance of intensity as a standalone factor - you can’t simply extend treatment time to compensate for low intensity.
For effective results:
- Superficial treatments typically require 20–50 mW/cm² with a fluence of 1–10 J/cm².
- Deep tissue applications demand higher intensities, around 100–200 mW/cm², with a fluence of 10–50 J/cm².
Exceeding these ranges can trigger the inhibitory phase, where too much light can actually reduce effectiveness - or worse, cause harm. As Michael R. Hamblin, Ph.D., from Harvard Medical School explains:
"A very low dose of light has no effect, a somewhat bigger dose has a positive effect until a plateau is reached. If the light dose is increased beyond that point the benefit progressively decreases... and further increases will actually start to have damaging effects on the tissue."
These parameters are the foundation for designing photobiomodulation devices that deliver precise and effective treatments.
Device Types and Technologies
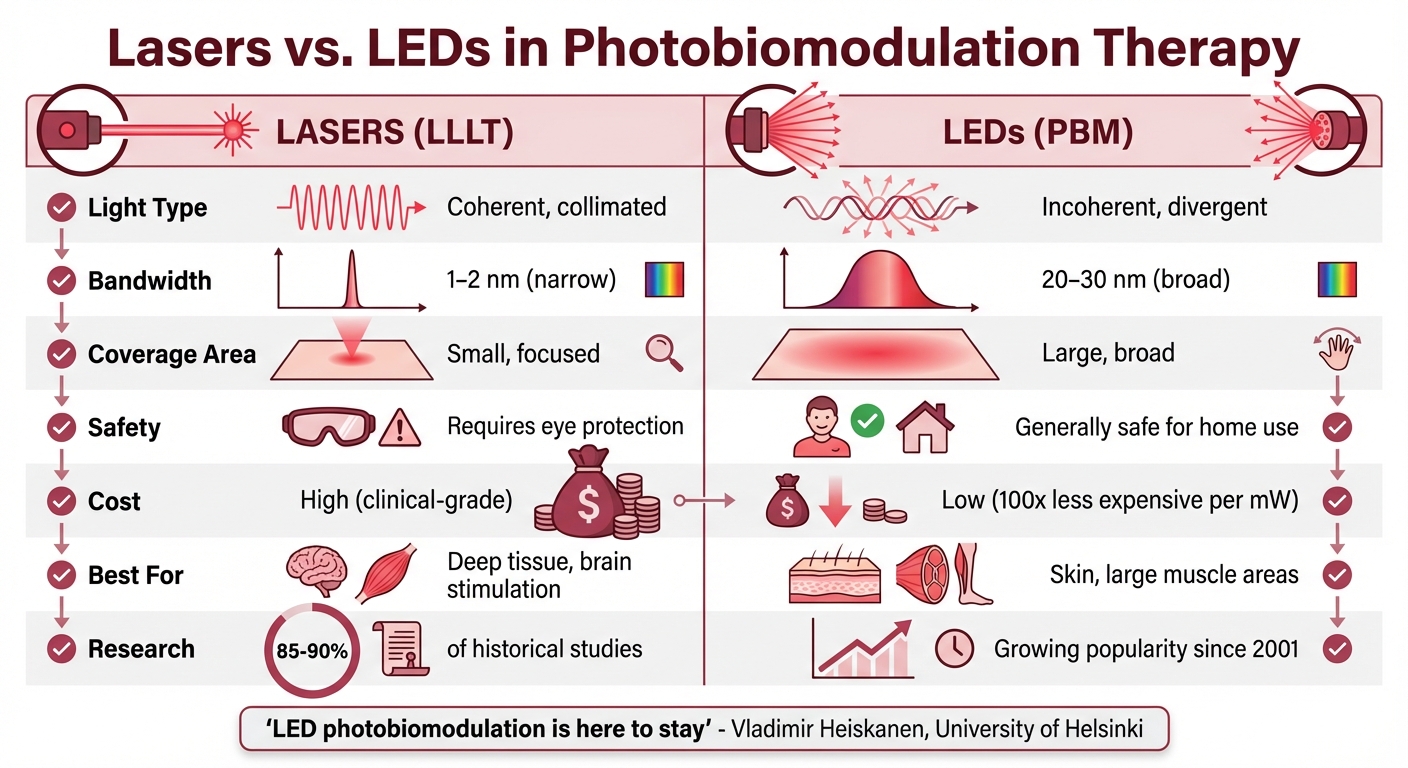
Lasers vs LEDs in Photobiomodulation Therapy: Key Differences
Photobiomodulation devices rely on either lasers or LEDs, each with distinct characteristics. These devices come in various formats, ranging from compact handheld units to full-body pods, each tailored to specific therapeutic purposes.
Lasers vs. LEDs
Let’s break down the key differences between lasers and LEDs in photobiomodulation (PBM) devices. The main distinction lies in how they generate and deliver light. Lasers produce light that is coherent, monochromatic, and collimated. This means the photons travel in synchronized waves with a narrow bandwidth (typically 1–2 nm), creating organized patterns known as "laser speckles." These speckles are about 1 micron in size, aligning with the dimensions of mitochondria. LEDs, by contrast, emit light that is incoherent and widely dispersed, with a broader bandwidth (usually 20–30 nm). The photons from LEDs travel in random waves, spreading out over a larger area.
Historically, lasers dominated PBM research, with 85–90% of studies focusing on laser-based devices. However, since 2001, LEDs have gained popularity due to their affordability and safety. LEDs are roughly 100 times less expensive per milliwatt of optical power compared to lasers. As Vladimir Heiskanen from the University of Helsinki aptly puts it:
"LED photobiomodulation is here to stay."
When it comes to clinical applications, the choice between lasers and LEDs depends on the treatment goals. For procedures requiring deep tissue penetration, like transcranial brain stimulation or deep joint therapy, lasers remain the go-to option. On the other hand, LEDs perform just as well for superficial treatments, such as skin rejuvenation and wound healing.
| Feature | Lasers (LLLT) | LEDs (PBM) |
|---|---|---|
| Light Type | Coherent, collimated | Incoherent, divergent |
| Bandwidth | 1–2 nm | 20–30 nm |
| Coverage Area | Small, focused | Large, broad |
| Safety | Requires eye protection | Generally safe for home use |
| Cost | High (clinical-grade) | Low (accessible for home use) |
| Best For | Deep tissue, brain stimulation | Skin, large muscle areas |
Safety also plays a critical role. Class III and IV lasers require protective eyewear and trained operators, while most LED devices are safe for home use. Heiskanen and Michael R. Hamblin highlight the advantages of LEDs:
"Advantages of LEDs include no laser safety considerations, ease of home use, ability to irradiate a large area of tissue at once, possibility of wearable devices, and much lower cost per mW."
Next, we’ll explore how these light sources are integrated into different device formats designed for targeted therapy.
Device Formats: Handheld, Panels, and Full-Body Pods
The design of PBM devices significantly impacts their usability and treatment scope. Different formats cater to various therapeutic needs, from localized care to systemic treatment.
Handheld devices are ideal for precise, targeted applications. They work well for dental treatments, trigger points, specific joints, or small wounds. Their compact design makes them perfect for addressing localized issues, leveraging the precision of lasers or LEDs.
Panels and arrays strike a balance between size and coverage. These devices, often equipped with LED grids, are effective for treating larger areas, such as muscle groups for exercise recovery or the face for skin rejuvenation. Some LED panels are even designed as wearable wraps, conforming to areas like joints or the abdomen for extended home treatments.
For those seeking whole-body benefits, full-body pods and beds are the solution. These clinical-grade systems provide systemic photobiomodulation, aiming to reduce inflammation, improve metabolic health, and enhance overall recovery. Specialized devices also cater to unique needs. For example:
- Helmets and caps support hair regrowth and transcranial brain stimulation, useful for conditions like traumatic brain injury or Alzheimer’s.
- Intranasal devices target systemic blood irradiation or neurological health.
- Transcranial devices using wavelengths like 1064 nm can penetrate up to 40 mm into the brain cortex, making them valuable for cognitive and neurological therapies.
Each format is designed with specific therapeutic goals in mind, ensuring that users can find a device suited to their needs, whether it’s localized treatment or full-body care.
sbb-itb-9616115
Benefits and Applications of Photobiomodulation
Photobiomodulation (PBM) offers a range of measurable health benefits. By tapping into natural cellular processes, it provides relief for pain, enhances skin health, and supports neurological function - all without the need for medications or invasive procedures. Let’s break down how this therapy works across different areas of health.
Pain Relief and Anti-Inflammatory Effects
PBM is highly effective in reducing chronic pain and inflammation. When red and near-infrared light penetrates tissue, it lowers levels of pro-inflammatory cytokines like TNF-α, IL-1β, and IL-6. It also inhibits the COX-2 enzyme, which reduces prostaglandin E2 (PGE2) - a key player in pain signaling. As Michael R. Hamblin from Harvard Medical School explains:
"One of the most reproducible effects of PBM is an overall reduction in inflammation, which is particularly important for disorders of the joints, traumatic injuries, lung disorders, and in the brain."
PBM promotes a shift in immune cells from a pro-inflammatory M1 state to a healing-oriented M2 state, accelerating tissue recovery. A 2007 study by Castano and colleagues demonstrated its effectiveness by treating rats with arthritis using 810 nm near-infrared light at 3 J/cm². After five days of treatment, knee swelling and serum PGE2 levels significantly decreased. Conditions like arthritis, fibromyalgia, and tendinopathies respond particularly well to this therapy. In 2020, researchers at the University of Arizona, led by Laurent Martin and Mohab Ibrahim, found that daily exposure to green light for 1–2 hours reduced pain intensity in patients with migraines and fibromyalgia.
These anti-inflammatory benefits also pave the way for improved skin healing and neurological health.
Skin Rejuvenation and Wound Healing
PBM works wonders for skin health by stimulating collagen production and speeding up wound healing. The therapy boosts ATP production, providing cells with the energy needed to multiply and migrate to damaged areas. This makes it particularly effective for treating chronic wounds like diabetic foot ulcers, venous ulcers, pressure sores, and even for facial rejuvenation and acne treatment. It also encourages the proliferation of gingival fibroblasts, which play a crucial role in wound closure.
When applied at specific high fluences, PBM can reduce skin fibrosis, improving overall skin texture and appearance. The shift in macrophages to the M2 phenotype creates an environment that supports faster and more effective healing.
But the benefits don’t stop at the skin - PBM’s ability to enhance cellular energy has systemic and neurological implications as well.
Neurological and Systemic Health Benefits
PBM can penetrate the skull to reach brain tissue, offering promising results for neurological conditions. It reduces neuroinflammation, protects neurons from excitotoxic damage, and promotes neurite growth and extension. For example, research led by Uri Oron found that applying near-infrared light to the tibia of transgenic Alzheimer’s mice once a week for two months improved cognitive function and spatial learning. The therapy activated mesenchymal stem cells, which helped clear β-amyloid plaques.
PBM’s applications extend to conditions like traumatic brain injury, Parkinson’s disease, stroke, and depression. In a 2021 study, participants with mild to moderate dementia who underwent daily PBM sessions for eight weeks experienced cognitive improvements.
| Benefit Category | Primary Mechanism |
|---|---|
| Pain Relief | Modulation of pain cells; NO release |
| Anti-Inflammatory | Reduced TNF-α, IL-6; M1 to M2 shift |
| Skin & Wounds | Increased ATP; collagen stimulation |
| Neurological | GSK3β inhibition; increased BDNF |
PBM also stimulates systemic healing. By mobilizing mesenchymal stem cells from the bone marrow, it helps repair tissues throughout the body. This "abscopal" effect means that treating one area can lead to benefits in distant tissues, making PBM a powerful tool for overall health and recovery.
Conclusion
Photobiomodulation (PBM) devices use targeted light therapy to kickstart cellular regeneration. By delivering red and near-infrared photons, these devices activate cytochrome c oxidase in mitochondria, setting off a chain reaction within cells. The result? Boosted ATP production, the release of nitric oxide, and a balanced response to reactive oxygen species. These cellular processes translate into practical benefits like reduced inflammation, faster wound healing, pain relief, and even neurological support.
With over 3,500 published studies and 1,000+ clinical trials backing it, PBM has a solid foundation in research. Its non-invasive and non-thermal nature makes it a standout compared to surgical lasers or pharmaceuticals. Instead of causing harm or introducing significant side effects, PBM works with the body’s natural healing mechanisms. As Michael R. Hamblin from Harvard Medical School explains:
"Photobiomodulation (PBM) involves the use of red or near-infrared light at low power densities to produce a beneficial effect on cells or tissues."
To get the most from PBM, it’s crucial to understand key parameters like wavelength (600–1100 nm), irradiance (5 mW/cm² to 5 W/cm²), and fluence (J/cm²). The "biphasic dose response" reminds us that dosing matters - too much or too little can reduce effectiveness, while the right amount stimulates healing.
Whether you're managing chronic pain, improving skin health, or supporting cellular vitality, PBM offers a natural, research-backed way to enhance well-being. Just be sure to choose devices with verified specifications and follow proper dosing guidelines for the best results.
FAQs
What should I know about safely using photobiomodulation devices at home?
When using a photobiomodulation (PBM) device at home, safety should always come first. The dosage - which includes how long and how often you use the device - needs to be tailored to your individual needs. Since everyone reacts differently, it's a good idea to start with shorter sessions and gradually adjust based on how your skin and overall well-being respond. This cautious approach helps minimize the chance of overexposure.
Always follow the manufacturer’s instructions closely, and if you’re unsure about anything or have specific health concerns, consult a healthcare professional. While PBM technology offers promising benefits, the science is still developing. To avoid potential risks like skin irritation or accidental eye exposure, it’s crucial to stick to established therapeutic guidelines.
How can I determine the right dosage and intensity for photobiomodulation therapy?
To figure out the right dosage and intensity for photobiomodulation therapy, start by clarifying your goal. Are you aiming to improve skin health, ease joint pain, or support muscle recovery? Each objective calls for specific light wavelengths. Red light (approximately 630–700 nm) is ideal for surface-level treatments, while near-infrared light (700–1,100 nm) reaches deeper tissues.
Look for a device with a power density between 5–200 mW/cm² to ensure effective energy delivery without risking overexposure. For most treatments, aim for a total energy dose of 4–10 J/cm² per session. You can calculate this by multiplying the device's power density by the session duration in seconds. For instance, using a device with 100 mW/cm² for 60 seconds delivers 6 J/cm², which falls within the recommended range.
Start with shorter sessions, around 2–3 minutes, and gradually increase the duration based on your tolerance and results. Most protocols recommend 3–5 sessions per week over a 2–4 week period, followed by a reassessment. Keep track of your progress by recording details like wavelength, session length, and frequency. This helps you stay consistent and adjust your approach if results taper off or if you experience mild irritation.
Can photobiomodulation support brain health and help with conditions like Alzheimer’s or depression?
Emerging research points to photobiomodulation as a potential way to support brain health and manage conditions such as Alzheimer’s and depression. This therapy appears to boost brain energy metabolism and lower inflammation - two critical aspects of maintaining neurological health.
Although early findings are encouraging, more clinical studies are necessary to establish its effectiveness. If you're considering this therapy, it's important to consult a healthcare professional to see if it aligns with your needs.
